Saturday, March 30, 2013
Friday, March 29, 2013
Leptospirosis in Dogs - Rat Fever
Leptospirosis is a highly
infectious bacterial disease that spreads via the urine of infected dogs or
rats. It can also spread to humans via contact from infected urine. The
bacteria initially enter, via contact with urine, into the blood stream and
travel to the animal’s organs such as the liver, kidneys, nervous system, eyes,
and reproductive organs.
Puppies are commonly more
susceptible than adults as their immune systems have not yet matured to be
strong enough to fight it off.
Cats certainly are exposed to leptospirosis,
and serologic studies indicate that infection occurs. But clinical disease is
rare. No specific disease syndromes have been associatedwith leptospirosis in
cats.
Causative agents
- Leptospira icterohaemorrhagiae
- Leptospira canicola
- Leptospira pomona
- Leptospira gripototyphosa
- Leptospira autralis
Transmission
Infected animals pass leptospira bacteria with their urine. Via contact
with infected urine or contaminated water the bacteria can enter other animals
through the mouth, eyes, open wounds, and skin abrasions. Transmission can also be the result of
an animal feeding on an infected organism or if the bedding is contaminated.
The bacteria thrive in humid and wet environments and so animals that enter the
water frequently are more prone to infection. Warm, stagnant and slow moving
water is an ideal breeding area for the leptospira bacteria. Some animals may
act as carriers without showing any clinical signs and so further transmission
may result.
Symptoms
 |
- High temperature
- Severe thirst
- Lethargy
- Vomiting
- Abdominal pain
- Dehydration
- Stiffness
- Jaundice
- Discharge from nose and eyes
- Frequent urination - may be followed by lack of urination
- Bloody diarrhea
- Liver failure (Leptospira icterohaemorrhagiae)
- Kidney failure (Leptospira canicola)
- Death often occurs in severe cases
- The diagnosis of leptospirosis may be difficult and a high proportion of infected pets may develop long-term infections.
- Blood tests and urine test can be used to give a positive diagnosis for leptospirosis.
- Serology is the most frequently used diagnostic test for dogs.
Treatment
Severe forms of the disease are
difficult to treat and can prove rapidly fatal.
- Tetracycline
- Fluoroquinolones - Ciprofloxacin
- Oral penicillin
- Administration of intravenous fluids
- If there is any liver or kidney failure then these will be treated accordingly.
Prevention
- Vaccination against leptospirosis
- Infected dogs should be kept away from healthy dogs
- Dogs should be kept away from stagnant waterways which may be the source of infection.
- Disinfection of kennels - Strong disinfectants should be applied to areas where the dog has urinated.
- Practice good hygiene including careful hand washing.
Human Disease
Wednesday, March 27, 2013
Cat Medication - How to give a pill
- Cat owners often face much difficulty with giving their cat a pill. Actually giving cat a pill may be a difficult process. There are some tips to make this process easier for both you and cat.
- Keeping calm is the key. Cats
are sensitive to nervousness, and they may become agitated. Never try to
medicate an excited or nervous cat. Therefore, you have to stay relaxed and
keep a positive outlook talking in a
soothing voice to your cat.

- Confine your cat to one room, placing it on a piece of carpeting: cats may want to grip the surface until they figure out what's going on. Spend for sometime petting, talking softly.
- Offer some cat food to attract the cat's interest.
- Have a large beach towel or blanket ready and wrap your cat in a towel, with the head protruding. This protects you and secures the kitty for easier handling.
- Snuggle the cat under your left arm, firmly against your body and hold its head in your left hand by its cheekbones. Though this may be an unpleasant experience for your cat, it's the most comfortable method of giving it needed pills.
- Before administration, get the pill ready and lubricate it with butter to make it ease in swallowing .
-

- Lodge the pill as far back on its tongue as you can.
- Quickly close its mouth and blow on its nose. The blowing will encourage it to swallow the pill.
- Stroke the chin and neck area gently, watching for signs of swallowing.
- Offer a small portion of a
treat or canned food to divert the cat's attention from ejecting the pill and
to ensure that the pill is indeed swallowed.

- Praise and reward the cat after the pill is administered, so the experience will be as positive as possible. Give the treat without the pill now and then, too.

Tuesday, March 26, 2013
Monday, March 25, 2013
Hazardous milk powder in Sri Lanka market
 A controversy has arisen with the
suspicion that milk powder containing DCD aka Dicyandiamide, a hazardous
agrochemical, has entered into the Sri Lankan market.
A controversy has arisen with the
suspicion that milk powder containing DCD aka Dicyandiamide, a hazardous
agrochemical, has entered into the Sri Lankan market.
The agro chemical was identified
in milk powder produced by New Zealand Dairy Company Fonterra whose flagship
brand ‘Anchor’ is widely popular in Sri Lanka.
New Zealand Government
investigation, according to their media, had revealed traces of soil- treatment
product DCD in 371 samples, affecting mainly milk powder. Traces have also been
found in one butter product and 11 cheese products.
New Zealand media also charged
that the country’s government did not know where the DCD-tainted products went,
although some would have been sold in New Zealand. This clearly indicates that
a large amount of milk powder products containing DCD have entered into the
markets where Fonterra is in operation, including Sri Lanka.
The amounts of DCD found in milk
powder products are contentious. Although some reports in New Zealand say
that the levels of DCD are “safe” and
mostly less than 1 part per million, some categorically assert that this poses
a serious threat to the public health.
DCD is a “nitrogen inhibitor” used
on pastures to reduce the harmful environmental effects of urea use and runoff
from cow effluent. It was revealed that Fonterra tests discovered the tainting
in September, but the public and export markets were not told until late
January. However, there is no internationally agreed acceptable level for DCD
in milk powder. In the wake of the revelation on DCD, Ravensdown and Balance
Agri-Nutrients, one of the biggest fertilizer companies of New Zealand,
withdrew the agrochemical from the market until acceptable residue levels have
been internationally agreed upon.
Although ‘The Nation’ attempted to
contact Leon Clement, Managing Director for Fonterra Brands in Sri Lanka,to ask
about the situation with regard to Fonterra milk powder brands in Sri Lanka, he
was not available to comment. However, Chairman of Pelawatte Dairy Industries
(Pvt) Ltd., and Mawbima Lanka Foundation, Ariyaseela Wickramanayake claimed
these tainted milk powder products may have found their way to the Sri Lankan
market. Among milk powder available in the Sri Lankan market, Lakspray,
Nespray, Ratthi and Anchor brands contain milk powder from New Zealand sources.
Officials of Nestle Lanka PLC
earlier told The Nation that ‘the quality of powdered milk products was checked
and approved by authorities of the respective countries where the items are
manufactured’ (‘Milk powder brands keep mum on ingredients’ in The Nation,
March 17, 2013).
Maliban milk powder is imported
from Australia while Pelawatte and Highland stand in the market as local
products.
Meanwhile, Trade Ministry
officials, in a statement on Friday, confirmed that samples of imported milk
powder would be sent abroad for testing to ascertain whether they had been
contaminated with DCD. The Ministry stated that the samples had to be sent
abroad as Sri Lanka did not possess the technical capabilities to conduct such
tests.
The controversy over DCD found in milk
powder surfaced following last week’s lead story of The Nation which revealed
that milk powder manufacturers were being vague when it came to listing the
ingredients in their milk products and their sources. This, as industry experts
explain, points out that the milk powder market in Sri Lanka should be highly
regulated by a state appointed body that has a wide mandate to rectify the
loopholes of the industry which put public health at risk.
What is DCD?
DCD is a nitrile derived from
guanidine. It is a dimer of cyanamide, from which it can be prepared.
2-Cyanoguanidine is a colourless solid that is soluble in water, acetone, and
alcohol, but not in diethyl ether or chloroform.
It is produced by treating
cyanamide with base. It is produced in soil by decomposition of cyanamide. A
variety of useful compounds are produced from 2-cyanoguanidine, guanidines and
melamine. It is also used as a slow fertilizer. Formerly, it was as a fuel in
some explosives. It is used in the adhesive industry as a curing agent for
epoxies.
Sri Lankan Market
New Zealand milk powder products
available in the Sri Lankan market
• Anchor
• Lakspray
• Nespray
• Ratthi
Australian milk powder products in
the Sri Lankan market
• Maliban
Local brands in the market
• Pelawatte
• Highland
The Nation
Sunday, March 24, 2013
Leptospirosis on the rise in Sri Lanka - Rat fever
The number of Leptospirosis (commonly known as rat fever)
cases island wide is on a sharp surge. With the exception of Jaffna, every
district has reported a rise in the number of suspected cases. The total number
of cases reported for this year is 858.
 According to the Government Epidemiology Unit (EPU,) 229
cases were reported islandwide in January, rising to 262 in February and up by
105 to 367 by March 21.
According to the Government Epidemiology Unit (EPU,) 229
cases were reported islandwide in January, rising to 262 in February and up by
105 to 367 by March 21.
At least eight districts have reported more than 50
suspected cases with Ratnapura (84), Anuradhapura (83), Kalutara (77),
Kurunegala (70), Polonnaruwa (65), Colombo (54), Gampaha (50) and Matara (50)
registering the highest number of reported cases. The districts with the lowest
incidence of cases are (2), Kalmunai (4), Puttalam (6) and Badulla
(9). Jaffna had no reported cases, EPU sources said.
Leptospirosis, a zoonotic disease endemic in Sri Lanka is
mostly found among those engaged in paddy farming. Chief Epidemiologist Dr.
Paba Palihawadana told the Sunday Observer that farmers had been advised to
keep their fields clean and ensure that accumulated water (following rains) is
flushed to eliminate rat urine prior to cultivation and to ensure their fields
are free of rat burrows.
March 23 2013
Saturday, March 23, 2013
Cameras on trains to minimize animal deaths
A pilot project was launched last week to minimize animal
deaths, especially of elephants, caused by collisions with trains at night.
The Department of Railways, with support from the private
sector, has taken the initiative of installing cameras on locomotives to
minimize the deaths of animals crossing rail tracks at night. The first phase
of the installation of these cameras took place at the Colombo Fort Railway
Station last week under the patronage of Transport Minister Kumara Welgama. The
night vision cameras will detect the movements of elephants or other animals
within the range of one kilometre.
Minister Welgama said depending on the success of the pilot
project, the Department will install a camera network on trains running on the
Northern rail track. The number of elephants dying following collisions with
trains has been increasing over the past few months. Ten elephants were killed
by railway accidents last year. The accidents have also caused massive damage
to the locomotives, in some instances even derailing trains. Sri Lanka Railways
has identified the areas between Kekirawa and Punani on the Batticaloa line,
between Galoya and China Bay on the Trincomalee line and between Maho and
Galgamuwa on the Anuradhapura line as most vulnerable for elephant accidents.
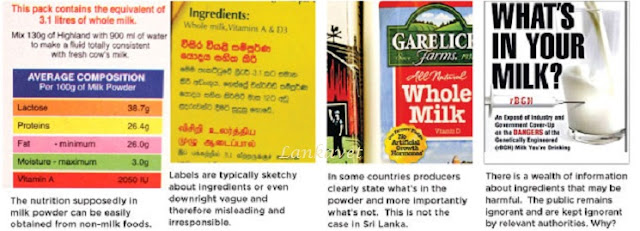
Milk powder brands keep mum on ingredients
Labeling laws are toothless:
Regulatory bodies lack machinery to check ingredients.
 In a backdrop where a
controversy looms large over the US dairy industry with regard to genetically
engineered growth hormones contained in milk powder , the Sri Lankan milk
powder industry lacks a mechanism to ascertain the ingredients and components
of the milk powder brands available in the local market.
In a backdrop where a
controversy looms large over the US dairy industry with regard to genetically
engineered growth hormones contained in milk powder , the Sri Lankan milk
powder industry lacks a mechanism to ascertain the ingredients and components
of the milk powder brands available in the local market.
In a survey done last week, The
Nation found that most milk powder manufacturers do not disclose or display the
ingredients contained in their products.
 While some contained the
substances, the sources of nutrients were also not specified. The officials
from various milk powder companies had a standard response to the questions
raised by The Nation. All of them said the products went through a number of
quality checks before it was put into the market. However, none of the
officials could provide a satisfactory explanation on the substances included
while producing powdered milk.
While some contained the
substances, the sources of nutrients were also not specified. The officials
from various milk powder companies had a standard response to the questions
raised by The Nation. All of them said the products went through a number of
quality checks before it was put into the market. However, none of the
officials could provide a satisfactory explanation on the substances included
while producing powdered milk.
Officials at Nestle Lanka PLC
told The Nation that the quality of powdered milk products were checked and
approved by authorities of the respective countries from where the items are
manufactured.
However, he pointed out that
most of its milk products are manufactured using locally obtained milk. “Over
50% of the products are from locally produced milk. Last year, our production
from locally obtained milk increased by 20%,” an official said.
Meanwhile, a senior research
officer at Maliban Milk Products (Pvt) Ltd said the powdered milk products are
certified and cleared by authorities in Australia, from where the company
imports powdered milk. “The products go through a series of checks where they
are manufactured. Our suppliers in Australia make sure that the products
conform to the requirements before they are sent,” the official said.
In addition, the official added
that the products are inspected by the likes of the Sri Lanka Standards
Institution (SLSI) and Medical Research Institute (MRI) once the items are
brought into the country. But, The Nation reliably learns that both the SLSI
and MRI lack robust machinery or mechanism to ascertain ingredients and
components of milkpowder.
Assistant Manager, Quality
Assurance at Milco (Pvt) Limited, Nilani Alwis, said the only ingredient in
their Highland milk powder packets was ‘milk’!
“There’s nothing else. We don’t
add chemicals or preservatives. We use spray drying method (a method of
producing dry powder from a liquid by rapidly drying with a hot gas)” she said.
She added their products were ‘100% local’ and were subject to stringent
quality tests. Hence, the public need not have any concerns, she stressed.
Meanwhile, Amal Wageesha,
Senior Lecturer in Biochemistry, Faculty of Medicine, South Asian Institute of
Technology and Medicine (SAITM) said that ‘Companies are bound by law to
display their ingredients, even if only one ingredient such as full cream milk
has been used. Most however, do use nutrients in an attempt to increase the
quality. At the most, milk powder contains a maximum of 3-4 ingredients, yet
manufacturers have a legal obligation to print these clearly’.
‘If the companies need to
survive without having legal action taken against them, they need to tell the
whole truth and disclose all ingredients,’ he added. However, during the survey,
The Nation found that such labeling laws are being murdered in broad daylight
by milk powder manufacturers.
Chairman of Pelawatte Dairy
Industries (Pvt) Ltd, and Maubima Lanka Foundation, Ariyaseela Wickramanayake
claimed that DCD (Dicyandiamide) Chemicals have been found in imported milk
powder. ‘Before that, there was the
Melamine scandal in China that killed several children and led to the execution
of those responsible following trials,’ he added. Wickramanayake further claimed that foreign
sub-grade milk is dumped in Sri Lanka to the tune of 83, 000 tons (in 2011).
rBGH, the hormone which is at
the centre of controversy, is injected into cows to increase milk production.
While approved by the FDA, the hormone is banned in Canada and the European Union
because of health risks to cows. Consumer advocates also say rBGH increases
levels of IGF-1, a hormone that’ is linked to prostate and colon cancer.
By The Nation
Sunday, 17 March 2013 02:29
Sunday, March 17, 2013
Saturday, March 16, 2013
Monday, March 11, 2013
Causes of Infertility in Cows & Buffaloes
Infertility in cattle accounts for major economic losses in dairy farming
and dairy industry. It becomes an economical burden to the farmers, since an
unproductive animal has to be maintained, and in most countries such animals
are driven to slaughterhouses.
Infertility describes as a temporary disturbance of reproductive function
in which cows or buffaloes fail to conceive and give birth to young ones. A healthy cow can normally produce a calf for
every 12-14 months interval.
 Also a cow should come to
estrus within 90 days after calving otherwise the calving interval is
prolonged. Infertility can be due to malnutrition, infections, congenital
defects, and ovulatory or hormonal imbalances. Infertility is also due to poor
management of calves resulting in delayed puberty and first calving. Therefore
good management practices should be adopted right from the calf hood.
Also a cow should come to
estrus within 90 days after calving otherwise the calving interval is
prolonged. Infertility can be due to malnutrition, infections, congenital
defects, and ovulatory or hormonal imbalances. Infertility is also due to poor
management of calves resulting in delayed puberty and first calving. Therefore
good management practices should be adopted right from the calf hood. Sterility is a total loss of
fertility and maintaining such animals is a waste and should be culled. Whereas
infertility is a temporary loss of fertility can be corrected if diagnosed in
the right time.
Sterility is a total loss of
fertility and maintaining such animals is a waste and should be culled. Whereas
infertility is a temporary loss of fertility can be corrected if diagnosed in
the right time.
The incidence of infertility is
more in buffaloes due to their seasonal way of breeding and poor regulatory
system of body temperature. Buffaloes require special management skills to
prevent infertility.
The causes of infertility are
many and can be complex.
Diseases of the genital organs
Infectious causes of infertility
- Trichomoniasis
- Brucellosis
- Vibriosis
- Leptospirosis
Physiological causes of
infertility
- Anoestrus
- Repeat breeding
- Cystic ovaries
- Silent heat
Anatomical causes of
infertility
- Fremartinism
- Hypoplasia of the ovaries and uterus or infantile genitalia
- Diseases of the genital organs
Sunday, March 10, 2013
Saturday, March 9, 2013
Safety of Drugs on Pregnancy in Dogs & Cats
A:
Probably safe. Although specific studies
may not have proved the safety of all drugs in dogs and cats, there are no
reports of adverse effects in laboratory animals or in women.
B:
Safe for use if used cautiously. Studies
in laboratory animals may have uncovered some risk, but these drugs appear to
be safe in dogs and cats or these drugs are safe if they are not administered
when the animal is near term.
C:
These drugs may have potential risks.
Studies in people or laboratory animals have uncovered risks, and these
drugs should be used cautiously, as a last resort when the benefit of therapy
clearly outweighs the risks.
D:
Contraindicated. These drugs have been
shown to cause congenital malformations or embryotoxicity.
|
Drug
|
Recommendation
|
Comments
|
|
Antimicrobial Drugs
|
||
|
Amikacin
|
C
|
Aminoglycoside
antibiotics easily cross the placenta and may cause 8th nerve toxicity or
nephrotoxicity.
|
|
Ampicillin
|
A
|
Crosses the placenta
but has not been shown to be harmful to fetus.
|
|
Amoxicillin
|
A
|
Crosses the placenta
but has not been shown to be harmful to fetus.
|
|
Carbenicillin
|
A
|
Crosses the placenta
but has not been shown to be harmful to fetus.
|
|
Cephalosporins
|
A
|
Crosses the placenta
but has not been shown to be harmful to fetus.
|
|
Chloramphenicol
|
C
|
May decrease protein
synthesis in fetus, particularly in bone marrow.
|
|
Ciprofloxacin
|
D
|
Do not use during
pregnancy, quinolones have been associated with articular cartilage defects.
|
|
Clavulanic
acid-amoxicillin
|
A
|
Crosses the placenta
but has not been shown to be harmful to fetus.
|
|
Clindamycin
|
A
|
Crosses the placenta
but has not been shown to be harmful to fetus
|
|
Cloxacillin
|
A
|
Crosses the placenta
but has not been shown to be harmful to fetus.
|
|
Dicloxacillin
|
A
|
Crosses the placenta
but has not been shown to be harmful to fetus.
|
|
Doxycycline
|
D
|
Tetracyclines can
cause bone and teeth malformation in fetus and may cause toxicity in mother.
|
|
Enrofloxacin
|
D
|
See ciprofloxacin.
|
|
Erythromycin
|
A
|
Appears to be safe
except for erythromycin estolate, which has been shown to increase the risk
of hepatotoxicity in women.
|
|
Gentamicin
|
C
|
Aminoglycoside
antibiotics easily cross the placenta and may cause 8th nerve toxicity or
nephrotoxicity. However, specific toxicities from gentamicin have not been
reported, and it may be used for a serious infection in place of a suitable
alternative.
|
|
Hetacillin
|
A
|
Crosses the placenta
but has not been shown to be harmful to fetus.
|
|
Kanamycin
|
C
|
Aminoglycoside
antibiotics easily cross the placenta and may cause 8th nerve toxcitity or
nephrotoxcitity.
|
|
Lincomycin
|
A
|
Crosses the placenta
but has not been shown to cause problems in fetus.
|
|
Metronidazole
|
C
|
Teratogenic in
laboaratory animals, but there is no information for dogs and cats. It
should be avoided during the first three weeks of pregnancy.
|
|
Neomycin
|
A
|
Not absorbed
sufficiently to cause systemic effects after oral administration.
|
|
Oxacillin
|
A
|
Crosses the placenta
but has not been shown to be harmful to fetus.
|
|
Oxytetracycline
|
D
|
Toxic to fetus and
may increase risk of hepatitis in mother.
|
|
Penicillin G
(benzyl
penicillin)
|
A
|
Crosses the placenta
but has not been shown to be harmful to fetus.
|
|
Streptomycin
|
D
|
Associated with
higher incidence of 8th nerve toxicity than other aminoglycosides. See
gentamicin.
|
|
Sulfonamides
|
B
|
Sulfonamides cross the
placenta and have produced congenital mal-formations in rats and mice,
but problems have not been reported in dogs or cats; in people, they have
caused neonatal icterus when administered near term. Avoid long-acting
sulfonamides.
|
|
Tetracycline
|
D
|
Tetracyclines can
cause bone and teeth malformations in fetus and may cause toxicity in mother.
|
|
Trimethoprim-sulfadiazine
|
B
|
Manufacturer states
that it is safe during pregnancy in
dogs.
|
|
Trimethoprim
|
B
|
Teratogenic in rats
but probably safe in other species. Folate antagonism and bone marrow
depression are possible with prolonged use.
|
|
Ticarcillin
|
A
|
Crosses the placenta
but has not been shown to be harmful to fetus.
|
|
Tobramycin
|
C
|
Aminoglycoside
antibiotics easily cross the placenta and may cause 8th nerve toxicity or
nephrotoxicity.
|
|
Tylonin
|
B
|
No information is
available.
|
|
Antifungal Drugs
|
||
|
Amphotericin-B
|
C
|
There are no known
teratogenic effects, but amphotericin is extremely toxic. Use only if
the disease is life threatening, in absence of a suitable alternative.
|
|
Griseofulvin
|
D
|
Teratogenic in rats;
causes multiple skeletal & brain malformations in cats.
|
|
Ketoconazole
|
B
|
Teratogenic &
embryotoxic in rats; antiandrogenic; stillbirths have been reported in dogs.
|
|
Miconazole
|
A
|
Apparently safe if
applied topically.
|
|
Antiparasitic Drugs
|
||
|
Amitraz
|
C
|
Manufacturer states
that reproduction studies have not been done; no information available.
|
|
Diethyl carbamazine
|
A
|
Manufacturer states
that the drug may be given to dogs throughout gestation.
|
|
Dithiazanine iodide
|
B
|
No information is
available; iodide salts may cause congenital goiter if administered for
prolonged periods during pregnancy.
|
|
Fenbendazole
|
A
|
Safe. Has been
administered to pregnant bitches without producing adverse effects.
|
|
Dichlorvos
|
B
|
Caution is advised
when administering cholinesterase inhibitors to pregnant animals, it should
not be administered to puppies or kittens, but studies in pregnant dogs and
cats suggest that there are not adverse effects during pregnancy.
|
|
Ivermectin
|
A
|
Safe.
Reproduction studies in dogs, cattle, horses, and pigs have not shown adverse
effects.
|
|
Levamisole
|
C
|
No information
available.
|
|
Mebendazole
|
A
|
Safe. In
reproduction studies in dogs, it was not teratogenic or embryotoxic.
|
|
Piperazine
|
A
|
Safe. No known
contraindications for the use of piperazine.
|
|
Praziquantel
|
A
|
Safe. No
adverse effects were seen when tested in pregnant dogs and cats.
|
|
Thiacetarsamide
(Caparsolate sodium)
|
No specific
information regarding toxicity to fetus is available. It can be
hepatotoxic and nephrotoxic, and heartworm adulticide should be postponed
until after parturition.
|
|
|
Bunamidine
|
A
|
Has been
administered to pregnant bitches without problems and is safe in pregnant
cats. Slight interference with spermatogenesis has been seen in male
dogs.
|
|
Pyrantel
|
A
|
Safe. Toxicity
studies have not shown any adverse effects.
|
|
Thenium
|
A
|
Safe.
Manufacturer states that except in young puppies, there are no known
contraindications.
|
|
Thiabendazole
|
B
|
Thiabendazole is not
teratogenic in laboratory animals, but high doses have produced toxemia in
ewes.
|
|
Trichlorfon
|
C
|
Caution is advised
when administering organophosphates to pregnant animals. Congenital
toxicoses have been reported following administration to pregnant sows.
Manufacturer states that trichlorfon should not be administered to pregnant
mares, but there are no recommendations for dogs and cats.
|
|
Anticancer Drugs
|
||
|
Doxorubicin
hydrochloride
|
C
|
May produce
malformations in newborn or embryotoxicity.
|
|
Azathioprine
|
C
|
May produce
congenital malformations but has been used in pregnant women safely. It
may be a suitable alternative to other drugs when immunosuppressive therapy
is required.
|
|
Chlorambucil
|
C
|
May produce
malformations in newborn or embryotoxicity.
|
|
Cisplatin
|
C
|
May produce
congenital malformations, embryotoxicity, or nephrotoxicity.
|
|
Cyclophosphamide
|
C
|
May produce
malformations in newborn or embryotoxicity.
|
|
Methotrexate
|
C
|
May produce
malformations in newborn or embryotoxicity.
|
|
Vincristine
|
C
|
May produce
malformations in newborn or embryotoxicity.
|
|
Analgesic Drugs
|
||
|
Acetaminophen
|
C
|
Safety not
established in dogs, toxic in cats.
|
|
Aspirin
|
C
|
Embryotoxicity has
been seen in laboratory animals but not in other species. Late in
pregnancy it may produce pulmonary
hypertension and bleeding problems.
|
|
Flunixin meglumine
|
C
|
Safety in pregnancy
has not been determined.
|
|
Gold
(aurothioglucose)
|
D
|
Laboratory animal
studies clearly show increased congenital mal- formations.
|
|
Ibuprofen
|
C
|
Safety in dogs and
cats not established.
|
|
Indomethacin
|
C
|
Can be toxic in
adult dogs; can cause premature closure of ductus arteriosus if administered
near term.
|
|
Phenylbutazone
|
C
|
Safety has not been
established. Long-term use can depress bone marrow.
|
|
Salicylates
|
C
|
Embryotoxicity has
been seen in laboratory animals but not
in other species. Late in pregnancy, it may produce
pulmonary hypertension and
bleeding disorders.
|
|
Anesthetic and
Pre-anesthetic Drugs
|
||
|
Acepromazine
|
B
|
Phenothiazines
should be avoided near term, they may produce neonatal CNS depression.
|
|
Atropine
|
B
|
Crosses the placenta
and has been used safely but may cause fetal tachycardia.
|
|
Butorphanol
|
B
|
Safe for short-term
use. Neonatal depression can be treated with naloxone.
|
|
Codeine
|
B
|
Safe for short-term
use. Neonatal depression can be treated with naloxone.
|
|
Diazepam
|
C
|
See anticonvulsants.
|
|
Fentanyl
|
B
|
Safe for short-term
use. Neonatal depression can be treated with naloxone.
|
|
Glycopyrrolate
|
B
|
Safe. Does not
cross placenta as readily as atropine. Studies in rats and rabbits have
not revealed teratogenic effects.
|
|
Halothane
|
C
|
Decreased learning
ability has been reported in rats after in utero exposure; depression may be
seen in neonates after cesarean section; excessive uterine bleeding may
be seen when administered during cesarean section.
|
|
Isoflurane
|
B
|
Probably safe.
Depression may be seen in neonates after cesarean section.
|
|
Ketarnine
|
B
|
Probably safe.
Depression may be seen in puppies delivered by cesarean section, may increase
intrauterine pressure and induce premature labor.
|
|
Lidocaine
|
A
|
All local
anesthetics appear to be safe when used for a local nerve block or epidural
anesthesia.
|
|
Meperidine
|
B
|
Opiates can produce
neonatal sedation and respiratory depression, but the effects can be reversed
with the administration of naloxone.
|
|
Methoxyflurane
|
C
|
Neonatal depression
is seen when used for cesarean section.
|
|
Morphine
|
B
|
Opiates can produce
neonatal sedation and respiratory depression, but the effects can be reversed
with the administration of naloxone.
|
|
Naloxone
|
A
|
Has been shown to be
safe when administered to newborns within a few minutes after birth.
|
|
Nitrous oxide
|
B
|
Probably safe. Used
frequently for cesarean section without adverse effects.
|
|
Oxymorphone
|
B
|
Opiates can produce
neonatal sedation and respiratory depression, but the effects can be reversed
with the administration of naloxone.
|
|
Pentobarbital
|
D
|
Associated with high
incidence of neonatal mortality.
|
|
Thiamylal
|
C
|
Easily crosses the
placenta; all barbiturates produce respiratory depression in fetus, however,
thiobarbiturates are not as toxic as pentobarbital.
|
|
Thiopental
|
C
|
Easily crosses the
placenta. All barbiturates produce respiratory depression in fetus; however,
thiobarbiturates are not as toxic as pentobarbital.
|
|
Gastrointestinal
Drugs
|
||
|
Antacids
|
A
|
Safe. Not
absorbed systemically.
|
|
Antiemetics
|
B
|
Probably safe if
administered short term.
|
|
Cimetidine
|
B
|
Safety has not been
established, but no reports of toxicity in humans.
|
|
Dimenhydrinate
|
B
|
Safe if used short
term.
|
|
Diphenhydramine
|
B
|
Safe if used short
term.
|
|
Diphenoxylate
|
C
|
Studies have
reported adverse effects in laboratory animals, but no adverse effects have
been reported in pregnant dogs, cats, and humans.
|
|
Laxatives
|
B
|
All laxatives,
except Castor Oil are considered safe if they are used short term.
Castor Oil causes premature uterine contractions.
|
|
Loperamide
|
C
|
Same comment as
diphenoxylate.
|
|
Metoclopramide
|
B
|
Safe in laboratory
animals, but no studies available for cats or dogs.
|
|
Methscopolamine
|
C
|
Safety not
established.
|
|
Misoprostol
|
D
|
Synthetic
prostaglandin, causes a termination of pregnancy.
|
|
Prochlorperazine
|
B
|
No reports of
toxicity when administered short term.
|
|
Ranitidine
|
B
|
Safety has not been
established, but no reports of toxicity were reported in humans.
|
|
Sucralfate
|
A
|
Probably safe.
Not absorbed systemically.
|
|
Sulfasalazine
|
B
|
Salicylate component
is not absorbed enough to produce adverse effects; sulfonamide may produce
neonatal icterus when used near term.
|
|
Cardiovascular Drugs
|
||
|
Atropine
|
B
|
Probably safe but
may produce fetal tachycardia.
|
|
Captopril
|
C
|
Has been shown to be
embryotoxic in laboratory animals and goats.
|
|
Digitalis
|
A
|
Probably safe.
No adverse effects seen in humans and laboratory animals.
|
|
Furosemide
|
B
|
No adverse effects
have been reported.
|
|
Dopamine
|
B
|
Probably safe at
therapeutic doses.
|
|
Heparin
|
B
|
Does not appear to
cross placenta.
|
|
Hydralazine
|
B
|
Probably safe.
There have been reports of minor toxicity in rats, but it has been
administered safely to pregnant women.
|
|
Isoproterenol
|
C
|
May cause fetal
tachycardia; beta-adrenergic drugs inhibit uterine contractions.
|
|
Lidocaine
|
B
|
Probably safe.
May cause fetal bradycardia.
|
|
Nitroglycerin
|
C
|
No information
available.
|
|
Nitroprusside
|
C
|
There is a risk of
fetal cyanide toxicity with prolonged use.
|
|
Procainamide
|
B
|
Probably safe.
May cause fetal bradycardia.
|
|
Propranolol
|
C
|
May cause fetal
bradycardia, respiratory depression, and neonatal hypoglycemia; avoid
use near term.
|
|
Quinidine
|
B
|
Probably safe.
May cause fetal bradycardia.
|
|
Theophylline
|
B
|
No reports of
adverse effects.
|
|
Thiazide diuretics
|
C
|
May cause increased
incidence of perinatal mortality.
|
|
Warfarin
|
D
|
Causes
embryotoxicity and congenital malformations, neural tube defects in
laboratory animals and humans.
|
|
Anticonvulsant Drugs
|
||
|
Diazepam
|
C
|
Has been associated
with congenital defects in mice, rats, and people.
|
|
Phenobarbital
|
B
|
Has been associated
with rare congenital defects and bleeding tendencies in newborn but may be
safer than other anticonvulsants
|
|
Phenytoin
|
C
|
Teratogenic in rats,
mice, and people.
|
|
Primidone
|
C
|
Same risks as
phenobarbital and has been associated with increased incidence of hepatitis
in adult dogs.
|
|
Valproic acid
|
C
|
May cause congenital
malformations.
|
|
Muscle Relaxants
|
||
|
Dantrolene
|
C
|
Safety not
established.
|
|
Dimethyl
tubocurarine
|
B
|
Quarternary base
with negligible placental transfer, it does not affect the fetus unless
administered in large doses.
|
|
Gallamine
|
B
|
Quarternary base
with negligible placental transfer, it does not affect the fetus unless
administered in large doses.
|
|
Methocarbamol
|
C
|
Safety not
established, manufacturer states that it should not be administered during
pregnancy.
|
Subscribe to:
Comments (Atom)




.jpg)



















.jpg)