

 For an abscess to occur, the pet must have been injured somehow. They are caused by obstruction of oil (sebaceous) glands or sweat glands, inflammation of hair follicles, or minor abrasions and punctures of the skin. Germs get under the skin or into these glands, which causes an inflammatory response as your pet's natural defense mechanisms kick-in to remove the foreign body.
For an abscess to occur, the pet must have been injured somehow. They are caused by obstruction of oil (sebaceous) glands or sweat glands, inflammation of hair follicles, or minor abrasions and punctures of the skin. Germs get under the skin or into these glands, which causes an inflammatory response as your pet's natural defense mechanisms kick-in to remove the foreign body.  To avoid being bitten and pounced on during kitty training, we have been using chopsticks and toothpicks to feed the kittens their treat. As seen in this video, this technique has worked particularly well with training "Gluteus," where the kittens will sit up straight, balancing on their buttocks muscles.
To avoid being bitten and pounced on during kitty training, we have been using chopsticks and toothpicks to feed the kittens their treat. As seen in this video, this technique has worked particularly well with training "Gluteus," where the kittens will sit up straight, balancing on their buttocks muscles.  Exocrine pancreatic insufficiency
(EPI) is a syndrome of maldigestion and malabsorption, caused by insufficient
synthesis and secretion of digestive enzymes by the exocrine portion of the
pancreas. It is much more common in dogs than cats. It is also referred to as
Pancreatic Hypoplasia or Pancreatic Acinar Atrophy (PAA).
Exocrine pancreatic insufficiency
(EPI) is a syndrome of maldigestion and malabsorption, caused by insufficient
synthesis and secretion of digestive enzymes by the exocrine portion of the
pancreas. It is much more common in dogs than cats. It is also referred to as
Pancreatic Hypoplasia or Pancreatic Acinar Atrophy (PAA).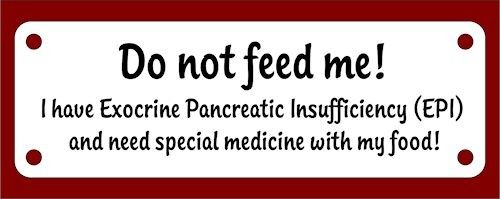







 Your dog will also continue to
be a contagion risk to other dogs for at least two months after the initial
recovery. You will need to isolate your dog from other dogs for a period of
time. Wash all of the equipments that your dog uses (e.g., dishes, kennel, toys)
with non-toxic cleaners. Recovery comes with long-term immunity against the
parvovirus, but it is no guarantee that your pet will not be infected with the
virus again.
Your dog will also continue to
be a contagion risk to other dogs for at least two months after the initial
recovery. You will need to isolate your dog from other dogs for a period of
time. Wash all of the equipments that your dog uses (e.g., dishes, kennel, toys)
with non-toxic cleaners. Recovery comes with long-term immunity against the
parvovirus, but it is no guarantee that your pet will not be infected with the
virus again. The way of transmission of this
disease to other animals is mainly due to ticks & fleas that have fed off
of other infected animals and in blood transfusions where infected blood from
one animal is transfused to an uninfected animal. When tick or flea suck blood
from your pet Haemobartonella are passed on. It can also be spread through fighting between
animals (body fluid exchange). In cats, the organism can also be spread from the
queen -mother cat- to her kittens.
The way of transmission of this
disease to other animals is mainly due to ticks & fleas that have fed off
of other infected animals and in blood transfusions where infected blood from
one animal is transfused to an uninfected animal. When tick or flea suck blood
from your pet Haemobartonella are passed on. It can also be spread through fighting between
animals (body fluid exchange). In cats, the organism can also be spread from the
queen -mother cat- to her kittens.
 A drop of blood is spread over
a microscope slide, stained and viewed microscopically; Haemobartonella may
appear in chains or as individual organisms across the surface of the red blood
cells. The number of organisms in the bloodstream can fluctuate dramatically.
There can be many observed in one sample, and a sample taken two hours later
may reveal none. Therefore; the blood smears should be made immediately after a
sample is collected. Haemobartonella felis
A drop of blood is spread over
a microscope slide, stained and viewed microscopically; Haemobartonella may
appear in chains or as individual organisms across the surface of the red blood
cells. The number of organisms in the bloodstream can fluctuate dramatically.
There can be many observed in one sample, and a sample taken two hours later
may reveal none. Therefore; the blood smears should be made immediately after a
sample is collected. Haemobartonella felis
 Puppies should not be separated from their mother before they are 8 weeks
old. Puppies that leave their mothers sooner have a rougher time adjusting and
a higher incidence of illnesses. It may be due to weakened
immunity or mourning the early loss of their family. Their mother's milk
provides them with the nutrition and immunity which needed to become healthy
dogs. At three to four weeks of age, puppies should begin eating some solid food. You
can try mixing three parts food with one part water or puppy replacement milk.
This will make the food easier to digest. If your puppy begins
eating a little solid food before it leave its mother it will have an easier
time adjusting when you bring it home.
Puppies should not be separated from their mother before they are 8 weeks
old. Puppies that leave their mothers sooner have a rougher time adjusting and
a higher incidence of illnesses. It may be due to weakened
immunity or mourning the early loss of their family. Their mother's milk
provides them with the nutrition and immunity which needed to become healthy
dogs. At three to four weeks of age, puppies should begin eating some solid food. You
can try mixing three parts food with one part water or puppy replacement milk.
This will make the food easier to digest. If your puppy begins
eating a little solid food before it leave its mother it will have an easier
time adjusting when you bring it home.
Breed
|
Weight
as an Adult Dog
|
Dry Food
|
Chihuahua,
Yorkshire Terrier, Toy Poodle
|
Up to 10
pounds
|
1/4 to ¾
cups
|
Miniature Poodle,
Scottish Terrier
|
10-25 pounds
|
3/4 to 1 cups
|
Cocker
Spaniel, Beagle,
Springer
Spaniel
|
25-50
pounds
|
1-2 cups
|
Collie, Boxer, Labrador,
Golden Retriever
|
25-50 pounds
|
2-2 ½ cups
|
Great
Dane, Malamute,
St.
Bernard, Mastiff
|
Over 75 pounds
|
2-4 cups
|